Clear the Clouds of Complexity Around Health Insurance
AI Fueling Healthcare Engagement and Well-being
Our verified solutions support tens of millions of lives, and our clients include Fortune 50 Market Leaders. Sensentia is revolutionizing the consumer and member experience by combining AI and innovative solution design. Our products are engineered to create transparency and efficiency while improving overall performance.
Up to 3x
Performance Gains
Verifiable increase in performance, speed to proficiency, elevated representative expertise, and thorough support in an instant.
30%
Cost Savings
Significant reduction in handle time and staffing needs through increased representative productivity and maximized efficiency.
99%+
Response Accuracy
Response inquiry precision and comprehensiveness to the point of legal liability. Our responses are always grounded, being tied to member contracts for auditability.
Sensentia AI Tools Deliver Accuracy, Comprehensiveness, and Accountability
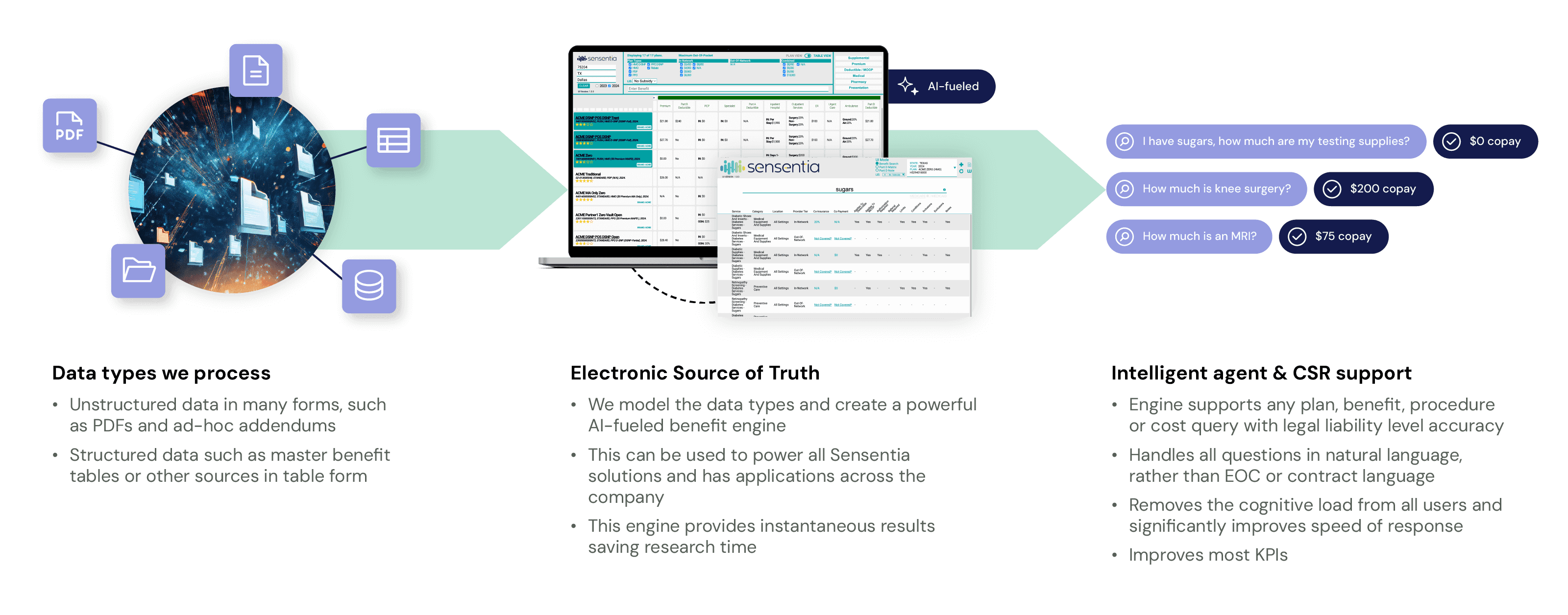
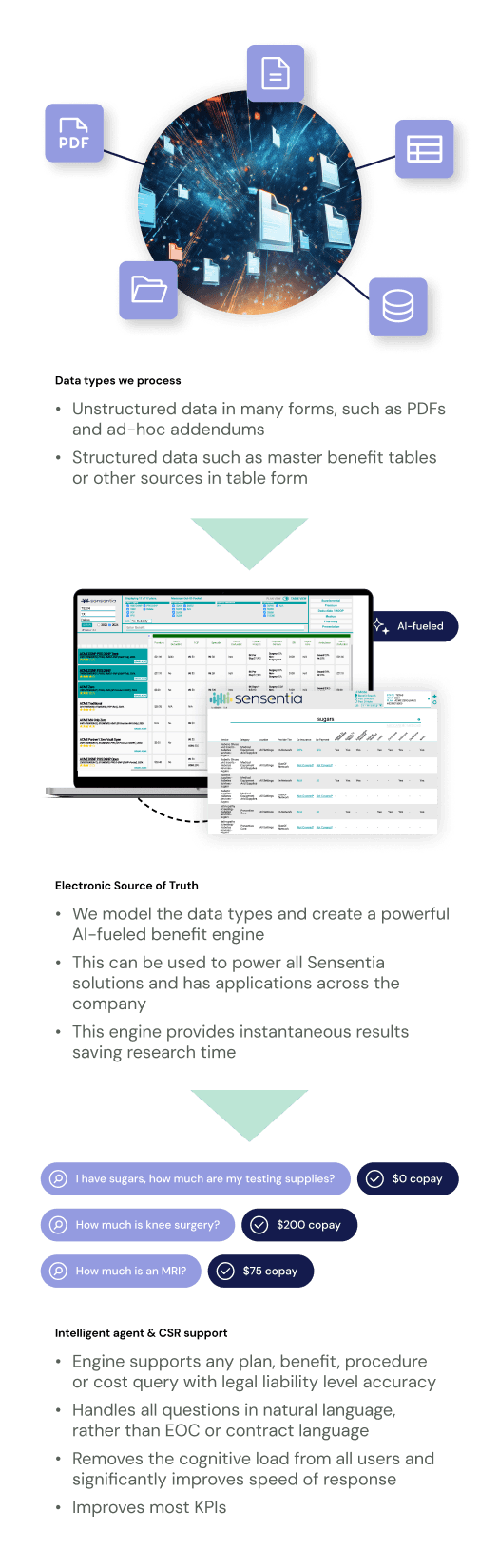
Our benefit tools are powered by our proprietary artificial intelligence, guaranteeing immediate, legally accurate, and comprehensive responses that differ from other approaches in the industry. Responses are directly tied to member contracts for all selected plans, ensuring full accuracy and reliability.
Members, CSRs, agents, and other users are usually unfamiliar with clinical and claims terminology, making it difficult to derive correct answers without natural language support. Sensentia’s systems reason and present information intuitively while supporting natural language, synonyms, and intent recognition during the query process.
Take a look at how Sensentia's innovative technology works when applied to a member portal.
Your One-stop Shop for Omnichannel Solutions
Our solutions integrate with any CRM and deploy through multiple channels to engage your consumers or members.
Web portal
Mobile app
Chat
Virtual assistant
Tablet
Call center

Exceed Targets at Reduced Costs for Sales Teams
Our innovative AI-fueled sales solutions significantly improve the shopping experience. We transform how prospective members shop and choose their ideal health plan.
Our benefit engine and customized interface design enable sales teams to deliver a seamless, optimized, and engaging shopping experience across all channels—whether selling in a contact center, on a website, or in the field.

Exceed KPIs at Reduced Costs for Member Service Teams
Our suite of AI-fueled benefit solutions greatly enhances the member experience, optimizing service delivery and boosting key metrics, including AHT, CSAT, NPS, first-call resolution, representative productivity, and onboarding.
Our customized benefit engine interface ensures a seamless and engaging service experience for members and providers regardless of their entry channels.

Get Ahead of the Curve: Achieve Compliance with Transparency In Coverage Rules
Our system ingests and calculates rates, presenting them in an easy-to-navigate member portal and benefit comparison tool. It’s grounded in member contracts, where costs are calculated rather than estimated and thus are indisputably accurate.
Consumers utilize our tools to research their cost-sharing responsibility across providers and locations. They can choose where to receive services at the lowest out-of-pocket cost. The results are full Transparency In Coverage Phase II and III compliance, better-informed members, and cost savings for carriers and members alike.

Enhanced Performance and Efficiency with Cost Savings for Carriers and TPAs
Sensentia's innovative solutions bolster productivity and reduce costs in various service and sales interactions provided by carriers and Third-Party Administrators.
We provide solutions for Transparency in Coverage Mandates, sales teams, service teams, and other departments that require intelligent plan/benefit data to provide improved services. Our benefit information is so accurate that we are trusted partners engaged to create Benefit Master Lists (BMLs) for our carrier clients - a source of truth for downline systems and processes.
Equip Your Team and Wow Your Customers
Keep your team happy
Provide immediate Q&A support to increase employee productivity and engagement while reducing panic, frustration, and turnover. No more combing through EOC docs or taking back-to-back calls with little hope of resolving customer concerns.
Train your CSRs and agents fast
Getting reps trained on Sensentia requires hours rather than weeks, boosting speed to proficiency and
positively impacting performance when scaling centers.
Make “buyer’s remorse” a rarity
Our system enables quick and easy multi-plan comparisons and compliant sales presentations, covering the benefits that matter. Buyers can be confident in their choices and experience less confusion.
Improve first-call resolution rates
Sensentia provides the answers your CSRs need to address customer inquiries quickly and confidently, eliminating the need for repeat calls.
Streamlined interface with an ingenious design
Our health plan benefit software is crafted to display tailored, role-specific information. Our UIs are customized to support efficiency, performance, and effectiveness, with easy-to navigate layouts that increase speed to proficiency and promote ease of use.
Information layout
Our information layout supplies users with precise information at the right time and in the right order for ease of use and understanding. Comprehensive information is just a click away.
Smart features
Fully supported functionality allows for quick and efficient searches with legal liability accuracy.
Easy integration
Easily integrate Sensentia tools with your existing CRM and applications.
The ultimate source of truth at your fingertips
Save time and money by eliminating manual research within SBs, EOCs, and Master Benefit Lists. Sensentia instantly delivers comprehensive benefit details to the forefront for easy and convenient reference and displays many of the calculations necessary for full service.
Comprehensive coverage details
Easily verify detailed procedure-level coverage details such as conditions, limits, inclusions, exclusions, and notes. Confirm copays, deductibles, and out-of-pocket maximums with a quick glance.
Tailored benefit views
View all plan-specific benefits based on the state, county, plan type, provider, place of service, and more.
Subsidy adjustments
Select the appropriate subsidy level and watch the benefit information update instantly.
Additional Sensentia Benefits
Reduced CTM and grievance rates
Sensentia reduces CTM and grievance rates by putting clear and accurate information at their fingertips. No more guesswork or response inconsistency.
Enhanced agent and rep expertise
Sensentia enhances agent and rep expertise by providing quick access to an indisputable source of truth tailored to their specific job duties.
Reduced turnover rates
Sensentia sets employees up for success and reduces turnover rates through technological innovations that are user-friendly, streamlined, and painstakingly accurate.
Improved speed to proficiency
Employee training on Sensentia solutions is done in hours—or even days—instead of weeks or months.
Enriched consumer experience
Due to enhanced information access, consumers receive top-notch member service and are empowered to shop with confidence.
Reduced system response time
Sensentia boasts a lightning-fast answer resolution time, especially as compared to benefit libraries.
FAQs
How do I improve sales performance?
Our SalesSense solution delivers an optimized shopping experience that supports agents and prospective members throughout the entire sales process. For sales teams, it will deliver increased overall sales and improved conversion rates on a “call to sale” or “lead to sale” basis. It will also reduce handle times, complaints, and turnover. With increased agent productivity, fewer staff members are needed to service the same volume of leads or calls YoY.
The lower staffing requirements and reduced handle time from increased productivity leads to savings that customers often use to pay for the solution and maintain budget parity.
How do I improve customer service KPIs?
Our ServiceSense solution delivers an optimized consumer experience that provides members or representatives with the support they need to receive or provide excellent service. For service teams, it will provide increased CSAT, NPS, accuracy and consistency of answers, first-call resolution, and representative productivity while significantly reducing handle time. As a result, teams will require less staff to service the same volume of calls YoY.
The lower staffing requirements and reduced handle time from increased productivity lead to savings that customers often use to pay for the solution and maintain budget parity.
How do I improve employee engagement and reduce turnover?
Employees often leave a position due to a lack of support or disparate processes that cause frustration. Our solutions provide support throughout the entire sales or service process, ensuring that answers to even the most complex questions are at employees' fingertips. By improving employee engagement, we avoid frustration, stress, burnout, and management escalations, all of which lower handling time and raise consumer confidence. Our system empowers employees to be experts and frees up management to provide sales or service stylistic coaching rather than answering numerous plan/benefit questions all day.
How do I improve Star Ratings or ratings in general?
Our innovative solutions significantly improve service quality, efficiency, and performance for sales and service teams. They relieve companies of the burden of improving their sales, retention, or service team performance, freeing up resources and investment for other segments. Customers respond positively when they are provided excellent service that supports them with informed decision-making.
How do I remove inconsistencies between sales and service segments?
When deployed across both sales and service teams, Sensentia's solutions use the same AI-fueled benefit engine and source data to ensure that sales conversations are supported in member conversations.
Our partners
Our APIs are developed to be user-friendly and robust, allowing for rapid integration with all major CRM systems.

Meet with one of our solutions experts today.
Unlock your team's true potential with Sensentia.