CompariSense: Powering personalized health plan selection with the latest in smart technology
Our intuitive platform guides consumers through a comprehensive needs assessment. It then instantly delivers unbiased, ranked health plan recommendations based on their specific upcoming medical needs, like a hip replacement or knee surgery.
CompariSense seamlessly integrates with your existing systems, whether as a self-service tool for your website or a powerful decision-support platform for your agents. Increase enrollments and cut millions in administrative costs with data-backed, error-free technology that meets the legal liability standard.

What you can expect with CompariSense
100%
Accurate, unbiased, data-backed plan recommendations
25%
Savings in agent compensation (new enrollments and renewals)
30-60 days
From kickoff to complete implementation
100%
Compliant responses that meet the legal liability standard
100%
Auditable decision process for complete transparency
24/7
Virtual support for any benefits questions
Better for enrollees and better for your bottom line
Health care plan selection is overcomplicated, costly, and inefficient. Agents are overwhelmed, consumers struggle with confusing choices, and self-enrollment rates remain low, leading to compliance risks, increased churn, and thousands spent on staffing and compensation costs.
With CompariSense, enrollment centers can finally offer an accurate, bias-free, and fully automated solution that ensures people choose the right plan at the right time, reducing rapid disenrolls and maximizing client lifetime value.
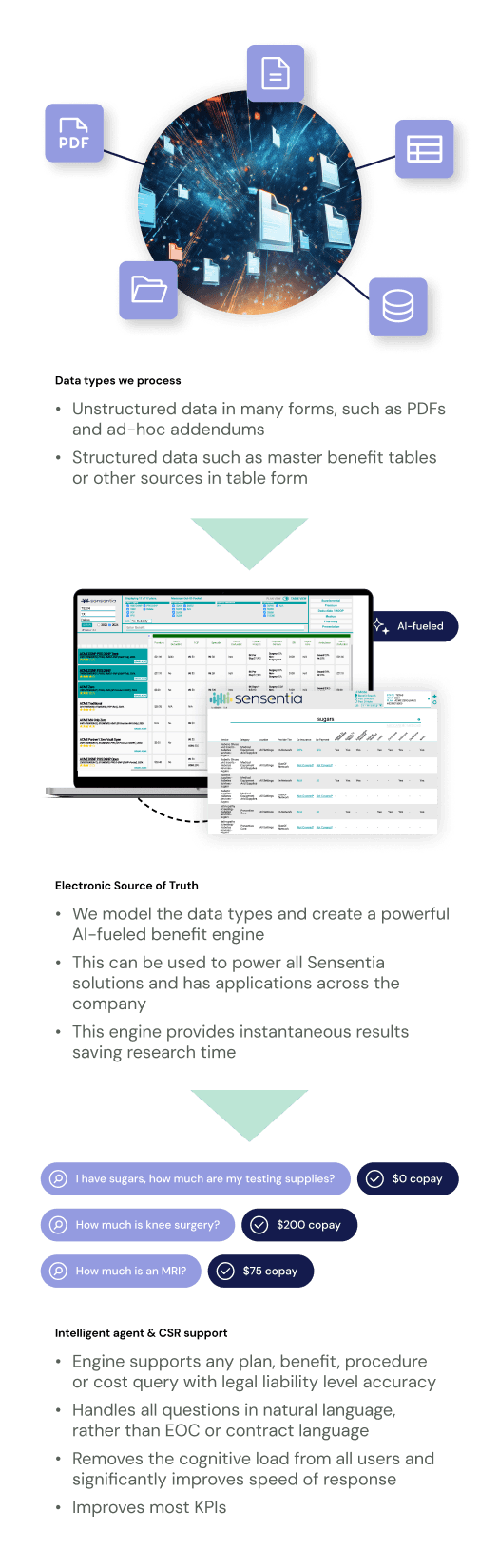
Sensentia Systems Deliver Accuracy, Comprehensiveness, and Accountability
Our benefit tools are powered by our proprietary artificial intelligence guaranteeing immediate, legally accurate and comprehensive responses different from other approaches in the industry. Responses are directly tied to member contracts for all selected plans, ensuring full accuracy and auditability.
Members, CSRs, agents, and other users are usually not familiar with clinical and claims terminology, making it difficult to derive correct answers without natural language support. Sensentia’s systems reason and present information intuitively while supporting natural language, synonyms, and intent recognition during the query process.
Take a look at how Sensentia's innovative technology works when applied to a member portal.
Increase your self-enrollment mix
CompariSense gives consumers the confidence to navigate plan selection independently, eliminating guesswork and confusion.
Step-by-step coverage assessment evaluates past and future healthcare needs to match people with the right plan
Unbiased, data-backed recommendations rank the best-fit plans first, ensuring a clear and easy decision-making process
Smart search delivers instant, legally compliant answers to plan questions and costs from the comfort of home, without agent pressure
Reduce post-enrollment complaints, increase customer satisfaction
Enrolling seniors in the right plan at the right time lowers member complaints while building trust and improving retention.
Smart technology eliminates human error and compensation bias, so that every recommendation is based solely on the consumer’s unique needs
Accurate plan matching prevents coverage surprises, reducing post-enrollment complaints and rapid disenrolls
Ongoing, on-demand virtual support leads to long-term satisfaction and higher revenue over the client lifetime

Support more enrollees without increasing staffing costs
CompariSense's round-the-clock virtual support guides customers through plan selection and beyond, cutting call volume and agent workload.
Plan selection AI handles an unlimited number of plan coverage, cost, and benefits questions
Program guidance AI provides real-time answers on Medicare, Medicaid, eligibility, and enrollment processes
Automated support reduces reliance on agents, reducing staffing and compensation costs
See CompariSense in action
What makes CompariSense different
Multidimensional plan ranking
Intelligent sorting prioritizes the best-fit plans based on real consumer needs, not sales incentives
Legally compliant and bias-free matching
Every recommendation meets the legal liability standard, ensuring transparency and compliance
AI-driven needs assessment
Leverages real-world customer insights to tailor plan recommendations with unmatched accuracy
24/7 virtual assistant support
AI provides instant, compliant answers to plan and benefit questions with no wait times, day or night
Enhanced consumer experience
Optimized self-enrollment improves plan selection accuracy and reduces member complaints
Fully white-label and customizable
CompariSense seamlessly integrates into your existing platforms, immediately enhancing your current workflow
Meet with one of our solutions experts today.
Unlock your team's true potential with Sensentia.
