Get Ahead of the Curve: Achieve Compliance with Transparency in Coverage Rules
Our AI-powered system ingests and synthesizes rates into an easy-to-navigate member portal and benefit comparison tool that’s grounded in member contracts and indisputably accurate.
Consumers can use it to research their cost-sharing responsibility across providers and locations. The result is full Transparency in Coverage Phase II and III compliance, better-informed members, cost savings, and much more!

Phase II & III full compliance
Positive impact on medical costs
CSR System or Member Portal compatibility
Why Transparency in Coverage Compliance is Crucial
Transparency in coverage is essential for improving the consumer experience, reducing costs, and enhancing consumerism in the healthcare industry. By addressing transparency gaps and achieving compliance with Transparency In Coverage rules, carriers and TPAs not only avoid sanctions and fees but improve the healthcare landscape for all.
Web portal
Mobile app
Virtual assistant
Tablet
Call center
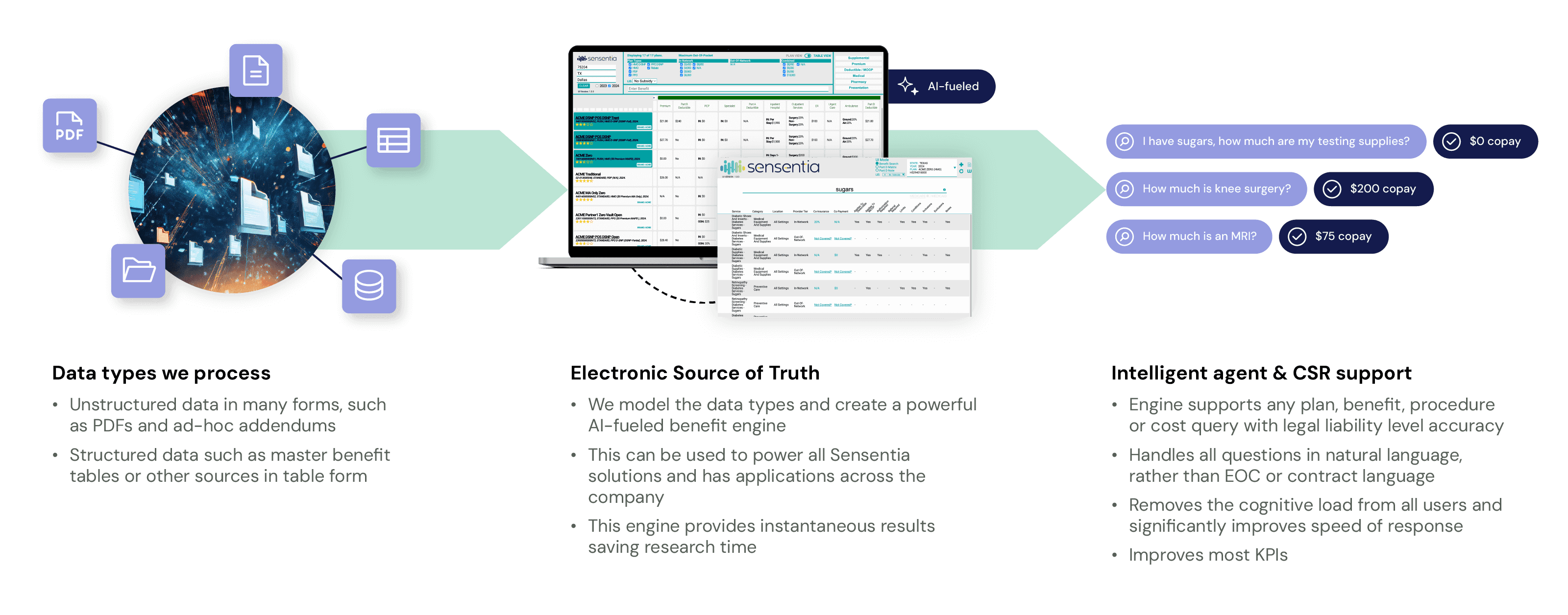
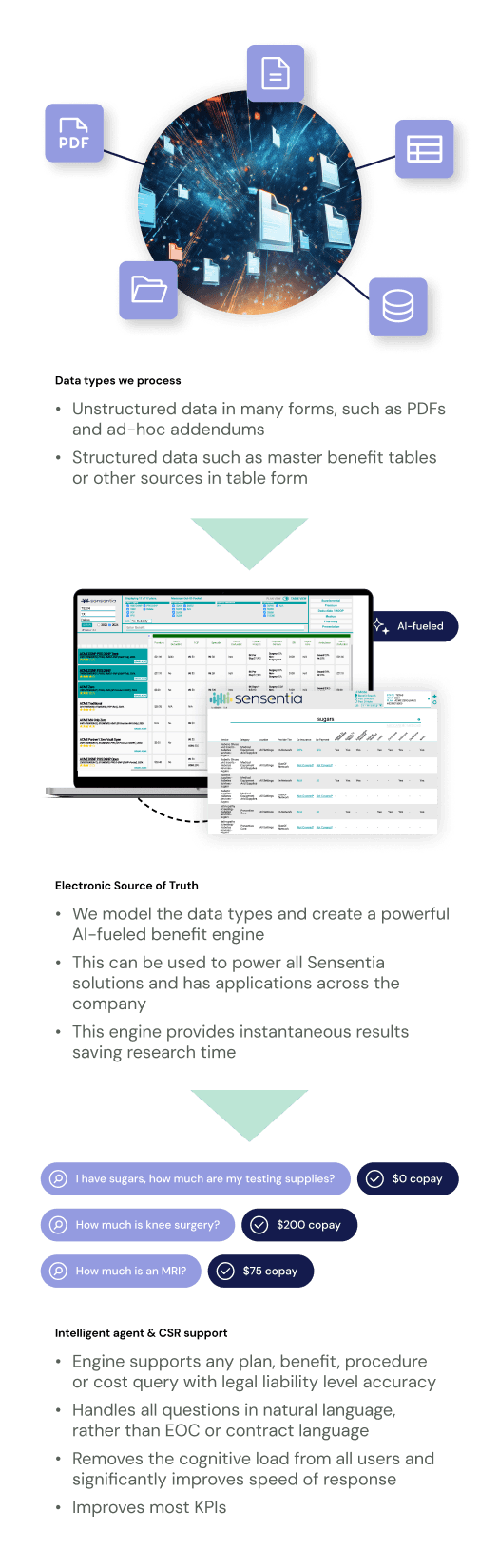
Sensentia AI Tools Deliver Accuracy, Comprehensiveness, and Accountability
Our benefit tools are powered by our proprietary artificial intelligence guaranteeing immediate, legally accurate and comprehensive responses different from other approaches in the industry. Responses are directly tied to member contracts for all selected plans, ensuring full accuracy and auditability.
Members, CSRs, agents, and other users are usually not familiar with clinical and claims terminology, making it difficult to derive correct answers without natural language support. Sensentia’s systems reason and present information intuitively while supporting natural language, synonyms, and intent recognition during the query process.
Take a look at how Sensentia's innovative technology works when applied to a member portal.
Access Done-for-You Compliance with Sensentia
Utilizing in-house resources to achieve compliance with Transparency in Coverage rules is a monumental challenge. Each stage requires substantial effort and resources:
Stage I: Produce machine-readable files containing contracted and allowable rates for items and services.
Stage II: Create an internet-based price comparison tool with personalized cost-sharing estimates for 500 items and services.
Stage III: Create an internet-based price comparison tool with personalized cost-sharing estimates for all items and services.
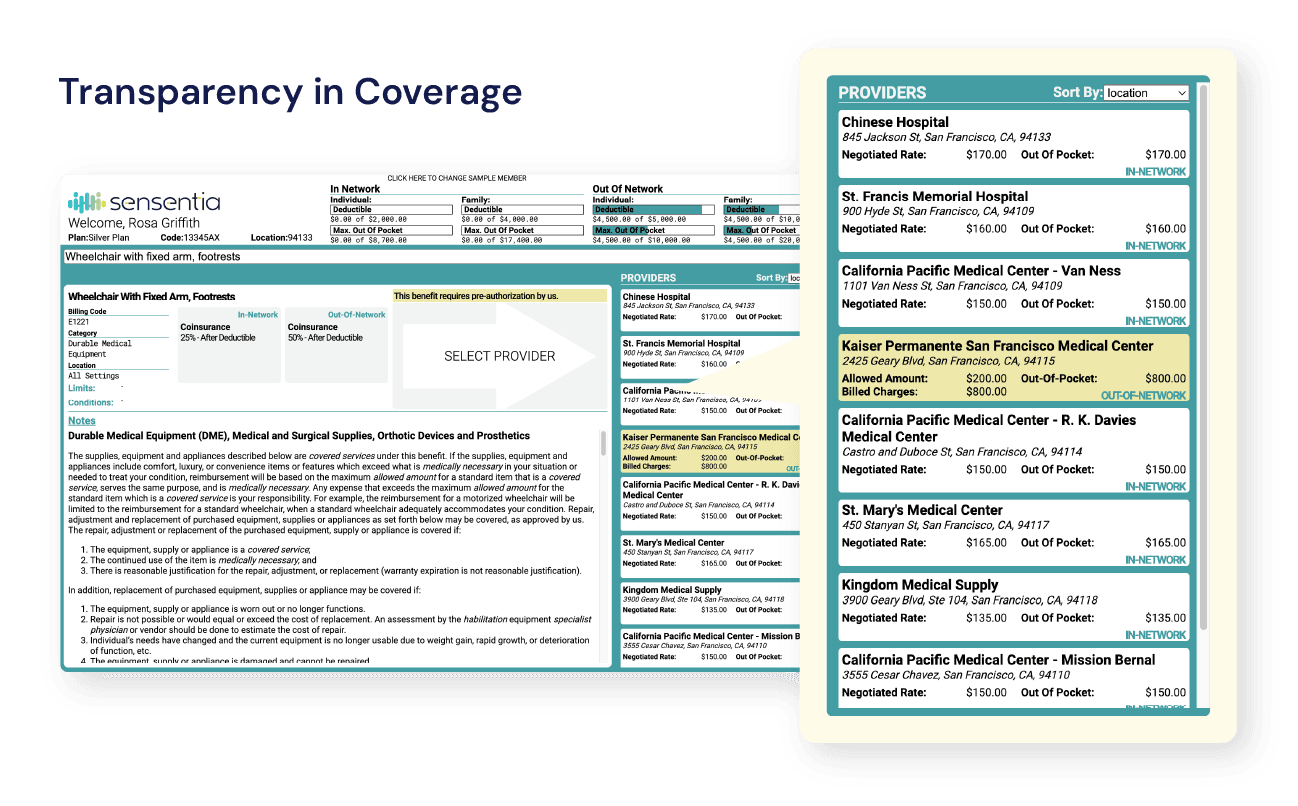
Centralized Member Portal with Comprehensive Benefit Information
With Transparency in Coverage by Sensentia, group health plans and insurers can provide members with a self-service tool that outlines all in-network and out-of-network cost-sharing information, including but not limited to:
Accumulators for out-of-pocket (OOP) and max out-of-pocket (MOOP).
Deductibles, copays, and coinsurance for specific services.
Applicable pre-authorization requirements.
Simple descriptions of selected services.
Real-Time, Legally Accurate Answers to Cost-Sharing Questions
Without information clarity and pricing disclosures, there’s no way for members to compare shoppable services and items. Sensentia’s AI engine synthesizes the information and makes it easily searchable by members. It enhances transparency and gives members real-time answers in seconds with just a few keystrokes.
Enter a query in the form of a code or plain language.
Click search.
View tailored benefits for that service or item.
Filter by location, provider name, and more to narrow the search results.
Stand Out Among Competitors and Elevate Success
A major pain point for members is a lack of transparency. Our innovative tools enable you to deliver an elevated user experience that puts clarity at the forefront and supports member autonomy. Sensentia differentiates your firm from competitors and fosters success.
Enhancing the customer experience breeds member loyalty, increases retention, and boosts revenues.
Abiding by regulations helps to improve your firm’s public reputation and legal standing.
Additional Transparency in Coverage Benefits
No guessing or surprises
The AI component of Sensentia never generates answers. All information is rooted in ingested member contracts and guaranteed to be accurate.
Smart filtering
Members can view benefits from multiple angles using filters that reorder and present information according to location, provider, and other parameters.
Easy benefit searching
Type the first three letters of a procedure and the system will populate potential procedure matches.
Reduced costs
Aside from helping you avoid financial penalties, Sensentia steers members toward lower-cost services and procedures, reducing costs for both the member and the carrier.
Tailored to everyday people
Members don’t have to know complicated clinical terms, as Sensentia understands plain language and synonyms for conditions and procedures.
Up-to-date information
All information Sensentia provides is up-to-date, guaranteeing the most accurate information possible.
FAQs
How can I ensure Compliance with TiC Mandates?
Sensentia's Transparency In Coverage solution fully complies with Phase II & III mandates and goes beyond by offering precise costs, considering all accumulators, instead of estimates. This aligns with the spirit of the 2023 No Surprises Act.
I'm in the Medicare LOB. What benefits would I receive by implementing this type of solution?
Whether or not you are required to comply with the Transparency in Coverage mandates, there is a large financial benefit to allowing consumers to see the out-of-pocket costs related to supplies or services in their area. For example, if you allow members to see the costs of a wheelchair or other DME from multiple suppliers in an area, your members will naturally choose the most economical source, which in turn benefits the member and the payor.
This type of cost-related utilization also benefits negotiations for payors, as it will create pricing competition among suppliers.
What timelines are involved with implementation?
Our solutions can be docked into existing CRMs or used as a stand-alone solution very quickly. Due to our simplified and easy-to-use interface, training time and speed to proficiency are reduced from days or weeks to hours. This is accomplished by removing the cognitive load from users, as all of our systems are fully supported by our AI-benefit engine, which provides natural language, synonyms, and intent logic. Depending on the state of the benefits data (structured or unstructured) and the sources of accumulator data (deductible, MOOP, etc.), we have launched systems in as little as 30 days.
Meet with one of our solutions experts today.
Unlock your team's true potential with Sensentia.